
- 04 Apr 2019
- Medical Revision
Dr Samuel Bourke, University of Birmingham Graduate and British army doctor, discusses the identification, causes and management of delirium from the viewpoint of a Junior Doctor.
“Hi Doctor – our post-op lady in bed 12 is being incredibly aggressive towards the nursing staff, she’s scratching us and has tried to bite me. Will you come and sedate her please?”. A common dilemma for young Junior Doctors, particularly overnight (due to the decreased number of staff), is the assessment of disoriented and aggressive patients. These patients, often elderly, can pose difficulties to nursing staff on the wards and their safety can often be compromised. The assessment and management of this cohort who frequently have a reversible underlying condition that alters their mental state, can often be incredibly challenging, and the implication of delirium in patients can have an impact on their morbidity and mortality.
What is Delirium?
Delirium is defined as “disturbed consciousness, worsening confusion, that is acute onset and fluctuating in nature, with an identifiable cause”, and is a huge problem in hospitals. It is often underdiagnosed, as it can be difficult to identify, and can have huge knock-on consequences for patients and healthcare systems. It results in an increased length of stay, and research has shown that it results in increased morbidity and mortality for patients. Witlox J et al.(1) have shown a 1.95x increased mortality in those with delirium compared to controls and a 2.41x increased risk of becoming institutionalised. There is a huge burden on the NHS, with an increased length of stay, and a further increase in the incidence of other conditions (e.g. infections, malnutrition).
Classically it is the elderly, frail patients who can present with delirium. However, this cohort is not exclusively affected. Those affected represent a spectrum, with those who are increasingly vulnerable requiring a smaller reversible “insult” to cause delirium. It is therefore important to not exclude the possibility of delirium, even in younger patients.
Identification of Delirium
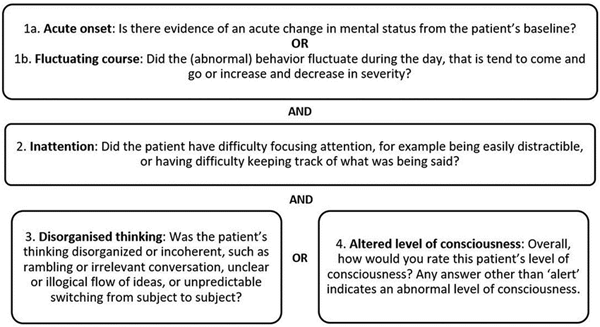
Delirium can often be difficult to identify, particularly for those of us who are relatively inexperienced. The Confusion Assessment Method (CAM) has been the most widely recognised, used and validated tool for the identification of delirium, however in my experience it can often take a long time, and requires a much more in-depth knowledge of the area to be able to use effectively. The 4AT, developed and validated in the UK for the detection of delirium, is a more straightforward and time-effective tool.
The Confusion Assessment Method (CAM)
Causes of Delirium
There are a wide variety of underlying causes of delirium, some of which are more common than others. A very common cause of delirium in post-operative patients is pain, and this should always be addressed. A helpful mnemonic which I came across whilst at Medical School, and that I found to be a useful mental checklist when assessing patients with delirium, was “PINCH ME”. It is a helpful tool to help guide your history, examination and investigations.
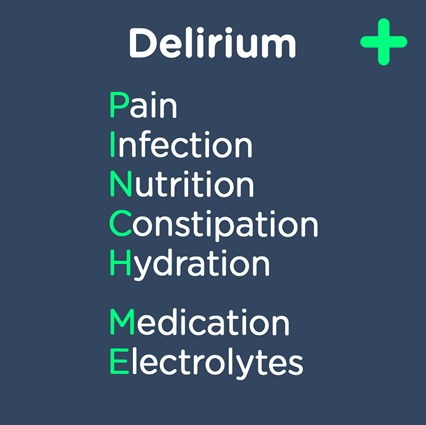
Remember – delirium is not a diagnosis. It is an essential first step to identify the presence of delirium, but it is much more important to attempt to get to the underlying reversible cause and address and treat this.
Management of Delirium
As we’ve touched on, the identification of delirium in the first instance, followed by the likely underlying reversible cause of the confusional state can be a challenge for FY doctors. The next challenge, and one that often arises at night when us Juniors are left to manage the wards on our own, is attempting to treat the cause and manage these patients. Systematically working through the most common causes of delirium as a checklist, and ensuring that a potential intervention is in place for each, would be a good start in the interim. Small steps are vital, including ensuring patients are adequately hydrated, have sufficient analgesia, or have had their bowels opened.
Experienced members of the nursing staff, particularly on elderly care wards, will employ a variety of techniques in the attempt to prevent delirium occurring in the first place. These include creating a familiar environment and encouraging friends and family to provide photos or familiar items to place around the bedside. Minimising disruption by ensuring that patients remain in the same bedspace is key, as well as ensuring their hearing aids and glasses are available and utilised.
A huge dilemma for junior doctors is whether sedation is appropriate in delirious patients who are being aggressive to members of staff, and who are potentially posing a risk to themselves as a result. It can be viewed as the easiest method to manage delirious patients, but can often have serious consequences. I personally have always been extremely reluctant to sedate these patients, and have only done so on one occasion. It should really be the last resort in their management, after as many different approaches to minimise agitation have been attempted. Unless absolutely required due to immediate danger to the patient or others, I would always advocate liaising with more senior members of your team before sedating any patients.
Delirium has huge implications for patients and the NHS as a whole and is often under-detected. A better understanding of prevention, identification and management can have positive effects for our patients.
(1) Witlox J et al. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. 2010 Jul 28;304(4):443-51.
Read the previous blog in this series: The NHS ePortfolio by Dr Samuel Bourke.
Dr Samuel Bourke, University of Birmingham Graduate and British army doctor.
- 04 Apr 2019
- Medical Revision
