
Dr Samuel Bourke, University of Birmingham Graduate and British army doctor, provides a guide to the NHS ePortfolio, including: reflections, discussions, clinical evaluations, and observations.
You’ve spent the last 5 or 6 years spending the vast majority of your time jumping through hoops and taking examinations, but now you’ve passed and have been let loose on the wards...
Those emails from the postgraduate coordinators about the importance of your new NHS ePortfolio are coming in thick and fast, and the last thing you want to do is sit down after a long day on-call and write a long-winded reflection. We’ve all been there and know the feeling.
What is the ePortfolio?
According to the NHS, an E-portfolio is an electronic tool doctors can use to log and record evidence that demonstrates their learning, achievements and abilities. The e-portfolio is an invaluable tool that can support FY1 Doctors in numerous ways such as:
- Helping to evidence your progress and learning
- Help you to think about your Personal Development Plan (PDP), encouraging you to think about what you need to do next to help you progress in your career
- Prepare for an interview for specialist studies
- Developing your CV
- Allowing you to reflect on your previous experiences and learn from previous mistakes to make future diagnoses
The ePortfolio, however, is the only “hoop” that you’ll need to jump through during your FY1 year, so taking an organised and methodical approach to your requirements can help prevent end-of-year stress about the dreaded Annual Review of Competence Progression (ARCP).
The Use Case of ePortfolio Reflections
Reflections form by far the largest component of the ePortfolio. Depending on what your respective trust deems their requirement (my trust for FY1 wanted us to complete 9 reflections minimum per rotation), the quantity can seem daunting if not completed regularly. Reflection itself is something that is omnipresent throughout the clinical years of Medical School and continues to play a vital role throughout foundation years, and both core and specialty training. As the Horus website states: “the skill of reflecting on your practice is vital in gaining a sense of how a method or actions can be improved upon”.
Recent issues have arisen surrounding the use of reflective pieces used as a source of evidence in criminal cases surrounding serious untoward incidents, as most famously highlighted by the recent conviction of Dr Bawa-Garba. 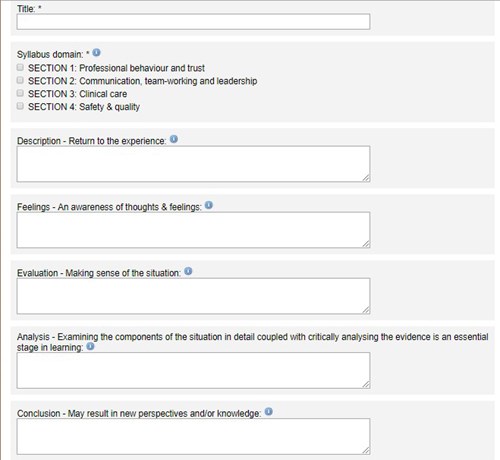
Despite this, the ability to reflect and analyse your actions at work, particularly in those cases or incidents that you have found particularly challenging, can be invaluable.
The reflections themselves are broken into a series of sub-headings; description, feelings, evaluation, analysis, conclusion and action plan. Although these are slightly arbitrary, they do provide helpful pointers and a template to reflect on.
Whilst the sheer number of reflections required can often result in a dilution in the quality of the reflections, I have found the ability to reflect on certain situations at work throughout my FY1 year particularly beneficial – particularly as a way to change the way I might approach certain situations, but most importantly as a way to decompress after emotionally draining cases.
The Value of Case-Based Discussions (CBDs)
In my opinion, CBDs help to form the majority of the educational opportunities that the ePortfolio can provide. Classically, interesting cases that require further learning outside of the hospital environment can be turned into a CBD. Asking a senior clinician at the time of a clinical scenario whether they would be willing to analyse a case-based discussion concerning what you have seen and witnessed is always helpful for learning.
There have been numerous cases throughout my FY1 year that have sparked a particular interest, or have highlighted gaps in knowledge, that provide useful material for further research.
Normally, only two CBDs are required per rotation. However, my advice would be to try to do one whenever you come across an interesting case that generates an area that requires a bit more research. They do not require a huge time commitment but do help with learning in a specific area of interest that will only help you in future practice should you come across similar patients or presentations again.
Mini-Clinical Evaluation Exercise (mini-CEX) and Direct Observation of Procedural Skills (DOPS)
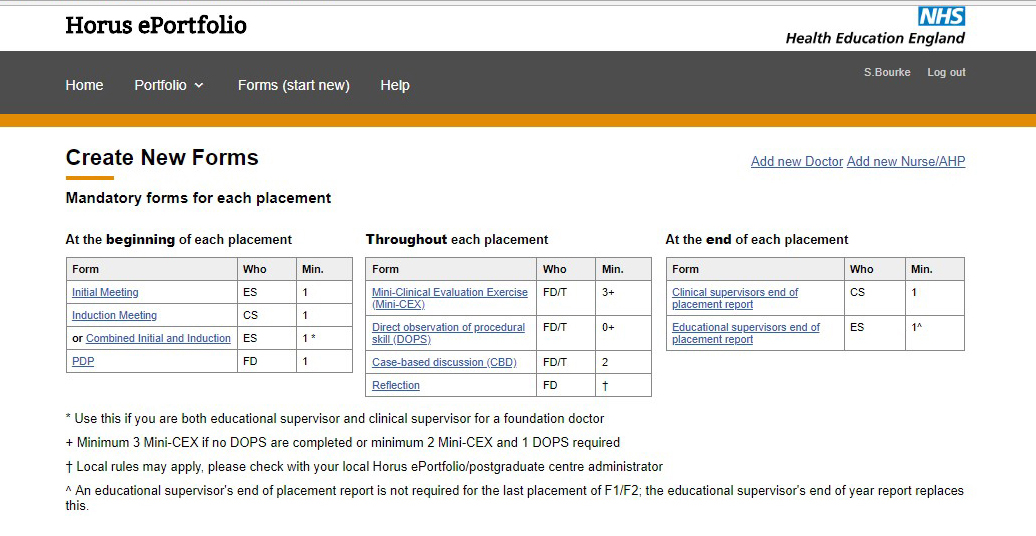
Mini-CEX and DOPS allow your seniors to analyse your clinical interactions. Although this is done on a day-to-day basis, the ePortfolio requires you to complete 3 mini-CEX per rotation (which can be decreased to 2 if you complete 1 DOPS). One of the best ways to get these done is usually in the setting of a ward round, where there are guaranteed seniors present, however, there are always other opportunistic settings.
Where the mini-CEX focuses on the communication between yourself and the patient, a DOPS looks at not only your communication but also your skills related to performing a practical procedure. This can be any procedure that isn’t one of the 15 core procedures that you are required to complete during your FY1.
Miscellaneous Others
- Core Procedures; there are 15 core procedures that you are required to complete under supervision throughout your FY1. These can be witnessed by a variety of the medical team, and in my experience, the majority of the procedures are witnessed by members of the nursing staff, rather than more senior doctors.
- Audit; one audit is required in each foundation year. There are also sections available to show involvement with quality improvement projects (QuIP). Getting an audit done during your first rotation not only relieves the burden towards the end of the year, but also enables you to try to present it at departmental meetings, and even gives the opportunity to re-audit at a later date.
- Team Assessment of Behaviours (TABs); this is usually completed at the end of the first rotation, and allows your supervisors to gain greater information about your performance at work, as well as your interaction with colleagues and patients. It is up to you to send TABS to a variety of members of the multi-disciplinary team (the ePortfolio dictates the breakdown of who you need to get TABs signed by, however, you are able to send more invites out than is needed), and also on you to chase up your colleagues to ensure that these are completed.
- SCRIPT modules; there are 15 compulsory eLearning modules on the SCRIPT eLearning website. Remember to save all the certificates as proof, to upload onto the ePortfolio.
The hardest part - tracking down your supervisor!
You will be given a Clinical Supervisor (CS) for each of your rotations, and your first supervisor will double up as your Educational Supervisor (ES) for the rest of the year. There is a requirement for an initial and end supervisor meeting for each of your rotations throughout FY1 and FY2, and therefore it is of huge importance to ensure that they are able to be tracked down. This can be a challenge with annual leave, or in certain specialties where Consultants are often tied up in theatre.
My advice would be stay organised and, particularly for the end of placement, get your meetings done as early as possible to avoid dramas with deadlines. This is particularly important when it comes to the ARCP (Annual Review of Competence Progression) at the end of the year.
The ARCP takes place halfway through the final rotation, meaning that you have slightly less time to get all of your required components completed over the final block. Not only that, but the ARCP dates often fall when supervisors may be taking annual leave, which can make the process even more stressful. The main way around this is to ensure that you have completed the vast majority of all the required sections significantly in advance, which will give you a much larger window to be able to sort the end-of-placement/year meetings out.
In summary:
- Get it done early
- Don’t be afraid to chase people to stay on top of things.

Dr Samuel Bourke, University of Birmingham Graduate and British army doctor.
- 04 Mar 2024
- Medical School